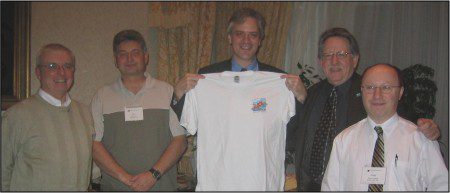
Go inside the Fletcher Science Lab at Brigham & Women’s with David Josephy and Dr. Jonathan Fletcher.
David Josephy is the President of Life Raft Group Canada, a member of the LRG Science Team, and the brother-inlaw of GIST patient Elsie Hernandez. David is a biochemistry professor at the University of Guelph, in Ontario. Since September, he has been on sabbatical leave, working as a researcher in the lab of Dr. Jonathan Fletcher, a renowned GIST researcher and leader of the Life Raft Group Research Team. We asked David to tell us about his experiences working at Brigham and Women’s Hospital in Boston.
Life Raft Group: “A sabbatical is like an extended vacation, right? (We asked, cheekily) “
David Josephy: “Hardly! I tell people that I’m now doing three fulltime jobs instead of my usual two. I’m still a faculty member in Guelph, with my own lab to run (by e-mail, mainly!) and I’m still helping out with the Canadian Life Raft Group. But now I’m also working every day in Jonathan’s lab in Boston.”
LRG: “So, starting with the science: we’d like to know what you are working on specifically, and we also want to know what’s new and exciting in GIST research?”
David:
 “Let’s start by giving some context for the Fletcher lab. Jonathan is an M.D. pathologist, and one of the strengths of his work is the close linkage between clinical medicine and basic science. He continues to do clinical diagnostic work, as well as lab research. It’s truly “translational” research – basic research with a close connection to medical practice. One of Fletcher’s special skills is the ability to grow cell lines from GIST tumors; most of the GIST cell lines used around the world started in his lab. The cells are grown under conditions where they continue to behave very much like the cells in the original tumors.”
“Let’s start by giving some context for the Fletcher lab. Jonathan is an M.D. pathologist, and one of the strengths of his work is the close linkage between clinical medicine and basic science. He continues to do clinical diagnostic work, as well as lab research. It’s truly “translational” research – basic research with a close connection to medical practice. One of Fletcher’s special skills is the ability to grow cell lines from GIST tumors; most of the GIST cell lines used around the world started in his lab. The cells are grown under conditions where they continue to behave very much like the cells in the original tumors.”
LRG: “So these cells have been removed from patients at surgery?”
David: “Yes. Several times, while I’ve been in the lab, tumor samples have been brought in from the operating room, and right away, Mark Mayeda or one of the other experienced people in the lab (not me!) puts them into culture medium. Most of the time, nothing useful starts to grow. Often, you just get fibroblasts or other non-GIST cells. But once in a while, GIST cells start growing and a cell line can be developed.”
LRG: “How do you know for sure that they are GIST cells?”
David: “It’s very similar to clinical pathology and diagnosis: you look at the appearance of the cells, and you use antibody stains to see which proteins they are expressing (producing), such as KIT and several others.”
LRG: “So you are growing GIST cells?”
David: “That’s right. I got trained on how to take care of the cells. It’s a bit like having a pet: you have to take care of them and feed them and they don’t know anything about holidays! The cells are grown in plastic flasks, fed three times a week, and “passaged” a few times each month.
LRG: “Fed? Passaged?”
David: “Feeding means changing the medium in the flasks; passaging means using enzymes to detach the cells from the flask, and then transferring them to new flasks. Just doing all the feeding and passaging for a large number of GIST cell lines, growing under a lot of different conditions, is a big part of the day-to-day work in the lab. All of the work has to be done in sterile conditions, in a flow hood, and you have to be careful all the time. Just brushing a pipette tip against your arm by mistake could contaminate a flask and ruin an experiment.”
LRG: “You sound like you are speaking from experience?”
David: “Actually not! So far, I haven’t managed to contaminate anything!”
LRG: “OK. Now let’s get back to our question: what you are working on, and what’s new and exciting in GIST research?”
David: “I’d highlight a couple of things: new technology and new targets – maybe leading to new drugs. Jonathan asked me to help with a large study called an “RNA pooled screen”. The idea is to make a “library” of GIST cells, where each library carries an extra little piece of DNA, a slightly different piece in each cell. The DNA causes the cell to make a little piece of RNA, and that in turn suppresses (that is, turns down without completely shutting off) the cell’s ability to make a specific protein. Each cell is a different “book” in the library, so it shuts down a different gene. Next, the cells are grown for a few months in the presence of a drug, such as Gleevec. Some of the cells – cells that are shutting down certain specific genes – grow faster under those conditions, and some grow more slowly. At the end of the experiment, we sequence DNA from the cells – it’s like making a catalogue of the library – and we identify the genes that have helped or hurt the cells. That way, we can identify possible new targets. Proteins that are helping the cells to grow, to overcome the effect of the drug, are probably proteins we want to attack, perhaps by using a second drug in combination with the first. So, I’m using this system to study one particular compound.”
LRG: “A GIST drug like Gleevec?”
David: “Well, it’s a compound that is being tested clinically in several cancers, but not yet in GIST.”
LRG: “And this is new technology?”
David: “Yes. The RNA interference screening technique has only been developed in the last five years or so. A lot of scientists are rushing to apply it to basic problems in cell biology and to improve therapies for HIV and for lots of different cancers. To make it work you have to be able to grow the cancer cells, and that’s where the Fletcher lab expertise is so critical. The DNA technology side of the study is done with the help of scientists at the Broad Institute, across the Charles River in Cambridge. We’ve been going over there a lot.
Related to this RNA interference technology, there’s also been an amazing improvement in the ability to catalog which genes are turned off or turned on in particular cells. Back in the 1990s, we studied gene expression by testing one gene at a time, now we can look at the entire human genome in one experiment. It’s like you’ve been working with a little pocket calculator for a few years and then suddenly you have a supercomputer sitting on your desk. A few months ago, this type of research turned up a previously unsuspected gene that is really important in GIST, a gene called ETV1, and a lot of people are now looking at ways to build on that discovery and devise new therapies for GIST.”
LRG: “How is your typical day in the Fletcher lab different from your typical day in your own lab in Guelph?”
David: “For me, it’s very different! Back in Guelph, I just sit in my office all day, doing paperwork and writing grants and talking to students… and teaching classes, of course. Here, I come to the Thorn building, put my backpack in a locker and my lunch in the fridge and then I spend the whole day in the lab, doing experiments and analyzing data – no phone calls, no committee meetings, no distractions. It’s great.
It’s also very different to be working in a hospital lab rather than a university campus. When you go to the cafeteria, the people you meet in the hallways are doctors, nurses and patients, not students. If you ever wonder what it’s all about, you can just walk along the “Pike”, the long corridor that connects all the buildings at Brigham and Women’s Hospital. You see the patients and you remember the reason why you’re doing the work.”