Monitoring is essential after diagnosis and surgery. Monitoring will help watch for recurrence or progression.
It is important to monitor GIST progression through imaging techniques. Magnetic resonance imaging (MRIs), Computed Tomography (CT) scans and Positron emission tomography (PET) scans have roles to play in the long-term surveillance of GIST, as well as determining response to drug treatments.
MRIs, CTs and PETs examined and clarified
Recently, concerns about exposure to radiation during scans have stirred significant discussion in the LRG email community. Although this is a decision that must be made between each individual and their treatment team, it is important to have a strong knowledge base when approaching the issue.
What is an MRI?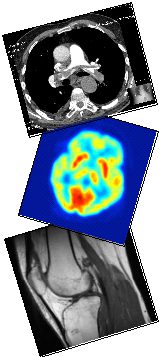
MRI stands for magnetic resonance imaging. Using a strong magnetic field, radio waves and acomputer, detailed pictures of tissue, bone and other internal structures are produced.
A doctor may request that a contrast material be utilized during the process; this may be either oral or intravenous. It is possible that an allergic reaction could occur from these substances. Kidney disease may also limit the use of contrast materials. The presence of some metals in the body (such as found in some defibrillators and other implants) may preclude the use of MRI’s.
Benefits:
• No exposure to radiation.
• May be able to better characterize and identify abnormalities and other focal lesions.
• May enable the detection of abnormalities that could be obscured by bone in other techniques.
• Contrast materials used in MRI’s are less likely to cause a reaction than contrasts used in other imaging techniques.
Risks:
• Patients that experience claustrophobia may require a sedative.
• Metals can interfere with the quality of the scan.
• Patients must remain perfectly still to ensure high-quality images. Breathing and bowel motion may cause artifacts or distortions when examining the chest, abdomen and pelvis.
• MRI’s are more expensive and take longer to perform than other techniques.
What is a CT scan?
Computed Tomography (CT) is a noninvasive test that may be used to diagnose and monitor many diseases. CT scans provide higher quality images of internal organs, tissue and blood vessels than x-rays. Specialized x-ray equipment produces multiple images of the body, called “slices”. A computer then joins the images into cross-sectional views that may be printed or viewed on a monitor.
Once again, a contrast material may be used during the procedure. A patient may be asked not to eat or drink anything for several hours before the exam. It is possible for some patients to have an allergic reaction to the contrast material since it contains iodine.
Benefits:
• High quality images may eliminate the need for more invasive testing.
• Images of bone, soft tissue and blood vessels may be produced simultaneously.
• Images are produced quickly and easily.
• Scans can be performed regardless of the presence of any implants.
• CT scans are less expensive than MRI’s.
• Scans are less sensitive to movement than MRI’s.
Risks:
• Exposure to radiation, although small, does occur. Cumulative exposure may be a concern.
• Allergic reactions are more common with the contrast materials used in CT scans, however they are still rare.
What is a PET scan?
Positron emission tomography, a PET scan, is a type of nuclear medicine imaging. This means that a small amount of radioactive material (called a radiotracer) is used during the exam. PET scans do not provide pictures or images of structures. The pictures produced by PET scans reflect the levels of chemical activity in different areas. Areas of greater intensity, or hotspots, indicate higher concentrations of the radiotracer and greater chemical activity.
The radioactive material critical for this type of imaging may be swallowed, injected or inhaled. This material collects in specific areas of the body and emits gamma rays, a type of energy. This energy is detected by a special device and a computer producing specialized pictures that demonstrate both function and structure of organs and internal structures.
PET scans measure blood flow, oxygen use and sugar metabolism. In GIST, the measurement of metabolism may provide a gauge of tumor activity or growth or response to treatment. Indolent GISTs may not be visualized accurately on PETs.
Benefits:
• The unique images produced provide information that may not be attainable using other techniques.
• Response to treatment may be measured.
Risks:
• The use of a radiotracer means exposure to radiation. It takes approximately 24 hours to leave the body.
• Allergic reactions may occur to the radiotracer.
• Diabetics may need to take special care when considering PET scans.
• Scans are time consuming and expensive.
• Resolution may not be as clear as in CTs or MRIs.
• Timing and scheduling are important to ensure accurate results.
 The role of CT and PET scans in the evaluation of GIST
The role of CT and PET scans in the evaluation of GIST
In the offices of the Life Raft Group, we receive reports of many CT scans findings that are inconclusive. On a regular basis, scans results are misinterpreted as resistance leading to the premature cessation of imatinib therapy which has the potential to reduce long-term survival. This is of greater concern when the radiologist reading the scans has little experience with GIST or when a patient is not consulting with a GIST specialist. Traditional criteria for the evaluation of tumor resistance are likely to over-diagnose the occurrence of progression. Proper use and interpretation of CT scans is vital for effective GIST treatment. Some experts in GIST imaging are now advocating the routine use of both CT and PET scans for GIST. At the present time however, CT (or MRI) is the recommended imaging method according to the NCCN sarcoma practice guidelines (v.1.2008). The guidelines also state to “Consider PET” and that “PET is not a substitute for a CT.” Proper use and interpretation of CT scans is vital for effective GIST treatment. Some experts in GIST imaging are now advocating the routine use of both CT and PET scans for GIST. At the present time however, CT (or MRI) is the recommended imaging method according to the NCCN sarcoma practice guidelines. The guidelines also state to “Consider PET” and that “PET is not a substitute for a CT.”
Initial response to therapy
Traditional RECIST criteria diagnose recurrence or progression based on an increase in tumor size or the identification of new lesions, either at the same site as the primary (a local recurrence) or at distant sites (metastases). Although an increase in tumor size is still important for identifying progression in GIST, the appearance of the tumor needs to be evaluated as well.
Frequently, the initial responses of GIST to imatinib therapy do not meet Response Evaluation Criteria in Solid Tumor (RECIST) guidelines for treatment response. GIST tumors may decrease in size slowly or only show a cessation of growth while responding well to treatment. In some cases, tumor size may increase due to hemorrhaging within the tumor, necrosis (tumor cell death) or tumor degeneration. How, then, can treatment success be evaluated?
PET Scans: When available, positron emission tomography (PET), using fluorine-18-fluorodeoxyglucose (18FDG) is an excellent tool for evaluating response. Unfortunately, due to cost and machine availability PET scans are not available to all patients. Alternatives for PET scans will be discussed later in this article.
If a doctor considers using PET to monitor therapy with Gleevec, Sutent or another tyrosine kinase inhibitor, a baseline PET scan should be obtained before the start of treatment. This provides a tool for comparison of future scans, allowing for evaluation of response.
Using PET scans, it is possible to observe responses to imatinib therapy in as little as 24 hours after initiation of treatment. Significant decreases in activity on PET scans can be seen within a month of starting imatinib therapy in patients that are responding to treatment. However, it may take appreciably longer for tumor shrinkage to appear on CT scans even when there is a strong benefit from treatment.
Those patients with primary resistance to imatinib therapy may also be identified using PET scans. These patients may show little to no decrease in activity on a PET scan. At this point it may be advantageous to consider alternatives to imatinib.
CT Scans: Although significant changes in tumor size may not be seen using computed tomography (CT), other changes in tumor characteristics make CT scans valuable in the evaluation of initial response. Tumor density changes may be visible in a single month following the initiation of imatinib therapy in responding tumors. Changes in density have been seen in as little as a single week. In addition to a decrease in tumor density, a decrease in vascularization may be seen. These changes have been shown to strongly correlate to activity reduction on PET scans. In contrast, using size alone may not show positive tumor response. In patients with primary resistance to imatinib therapy, changes in tumor density and vascularization may not appear indicating a need to explore alternative therapies.
GIST liver metastases that are responding to treatment may become more cystic during imatinib treatment and therefore more visible on a CT scan. Some lesions may not be visible on a CT scan prior to initiation of imatinib therapy and appear as they respond to treatment. Care must be taken not to misinterpret these findings as progression and prematurely cease imatinib therapy.
Long-term surveillance of tumor response
Both CT scans and PET scans have roles to play in the long-term surveillance of GIST response to imatinib. Traditional RECIST criteria diagnose recurrence or progression based on an increase in tumor size or the identification of new lesions, either at the same site as the primary (a local recurrence) or at distant sites (metastases). Although an increase in tumor size is still important for identifying progression in GIST, the appearance of the tumor needs to be evaluated as well.
CT scans: As mentioned earlier, it is important to evaluate the density and vascularization of a GIST tumor when evaluating progression. Changes in size without changes in these other tumor characteristics may not indicate progression. In addition, it is possible for a GIST tumor to develop intratumoral (within the tumor) nodules when secondary resistance first begins developing. An intratumoral nodule will appear as change in density and structure.
PET scans: PET scans are very useful for identifying the onset of secondary resistance. When the results of a CT scan are inconclusive or inconsistent with clinical observations, a PET scan may help clarify the situation. When secondary resistance develops, an increase in activity is seen on a PET scan. The use of PET scans may help with early identification of progression as well as prevent misdiagnoses of progression.
Both PET and CT scans are valuable tools in the evaluation and surveillance of GIST. Traditional RECIST criteria may over-diagnose primary resistance and progression. When available, PET scans are an excellent tool for clarifying questionable scans. However, when PET scans are not feasible, evaluation of additional tumor characteristics such as density may help reduce the misdiagnosis of resistance.
Please note that while current practice often involves physicians prescribing more frequent scans up front in a patient’s treatment and then tapering off their use later, some prominent clinicians, such as Heikki Joensuu, believe this is not optimal, but instead call for a different frequency of scans. Please click here to see a post that links to an article from Dr. Joensuu that explains this in further detail.
References
Benjamin RS, Choi H, Macapinlac HA et al. We Should Desist Using RECIST, at Least in GIST, J Clin Oncol 2007;25:1760–1764.
Choi, Haesun. Response Evaluation of Gastrointestinal Stromal Tumors, Oncologist 2008 13: 4-7; doi:10.1634/theoncologist.13-S2-4.
Demetri GD, von Mehren M, Blanke CD et al. Efficacy and safety of imatinib mesylate in advanced gastrointestinal stromal tumors, N Engl J Med 2002; 347:472–480.
Van den Abbeele, Annick D. The Lessons of GIST–PET and PET/CT: A New Paradigm for Imaging, Oncologist 2008 13: 8-13; doi:10.1634/theoncologist.13-S2-8, NCCN Sarcoma Practice Guidelines in Oncology – v.1.2008.
Demetri, Benjamin, Blanke, et al., NCCN Task Force Report: Optimal Management of Patients with Gastrointestinal Stromal Tumor (GIST Update of the NCCN Clinical Practice Guidelines, Journal of the National Comprehensive Cancer Network, Volume 5, Supplement 2.
H. Joensuu, et al, Follow-up strategies for patients with gastrointestinal stromal tumour treated with or without adjuvant imatinib after surgery. Eur J Cancer. 2015 May 25. pii: S0959-8049(15)00395-0. doi: 10.1016/j.ejca.2015.05.009.
